| OVERVIEW Patients with adrenal histoplasmosis may present in adrenal failure or more often with an enlarged adrenal gland, unilateral or bilateral. Symptoms have usually been present for between one to six months, or patients are asymptomatic. A minority present with adrenal failure, with weight loss, fatigue, anorexia and (importantly) low-grade fever. Pain and a sensation of heaviness in the abdomen with weight loss is a relatively common presentation. Many patients have lesions at other sites, such as the mouth, skin or GI tract. Hepatosplenomegaly is absent. For more information see Gajendra et al, 2016. |
| FUNGI Histoplasma capsulatum (and its new sibling species Histoplasma mississippiense, Histoplasma ohiense and Histoplasma suramericanum) |
| GLOBAL BURDEN Patients are described wherever histoplasma is endemic, or have travelled to endemic regions, as it presents years after exposure. |
| RISK FACTORS Adrenal histoplasmosis is very rare in acute disseminated histoplasmosis. It is found in non-immunocompromised people, typically over the age of 40 years. Diabetes is a common co-existing condition. |
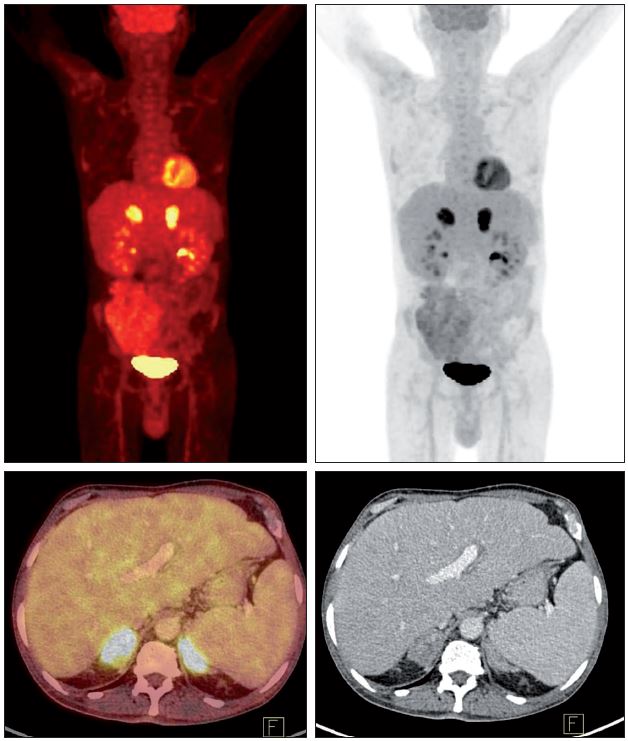
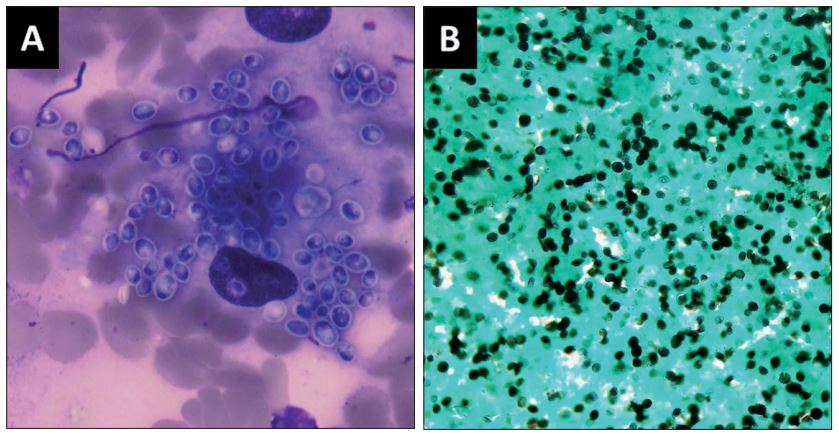
| DIAGNOSIS CT imaging of the adrenal glands shows either generalised enlargement or a nodule within one or both glands. Central hypodensity and peripheral rim enhancement of the adrenals are common and found only in histoplasmosis and tuberculosis. Adrenal function should be assessed with an adrenocorticotropic hormone stimulation assay. The definitive diagnosis is achieved with either ultrasound-guided fine needle aspiration or biopsy of the enlarged adrenal gland, with direct microscopy or histopathology. Typical small intracellular yeasts are visible in tissue. Cultures are rarely done. Serum histoplasma antibody is often positive but cannot be used to rule the diagnosis out. |
| TREATMENT Itraconazole 200mg or 400mg daily is highly effective. Often patients have been empirically treated for tuberculosis first (which can precipitate adrenal failure because of accelerated metabolism of cortisol) and a three-week delay after stopping rifampicin is required to allow itraconazole levels to be therapeutic. Careful supervision is required for patients with adrenocortical dysfunction or failure. |
| OUTLOOK The outlook is good. Antifungal therapy cures the disease. Patients with significant co-morbidities may not do as well. |