Factsheet
| NAME Talaromycosis, Talaromyces marneffei infection (formerly Penicilliosis) |
| FUNGI RESPONSIBLE Talaromyces marneffei |
| DISEASE In those with AIDS, most patients have fever, weight loss and malaise. Subcutaneous abscesses and papule-like ulcers are common. Sometimes the skin lesions are very small, like molluscum contagiosum. Anaemia, hepatosplenomegaly, lymphadenopathy and diarrhoea are also relatively common. As patients usually have very low CD+ counts, other concurrent opportunistic infections are common. Cough is common, but pneumonia is rare, despite this being the portal of entry of the organism. Patients can occasionally present in a confused state, with abnormal cerebrospinal fluid findings. In non-HIV patients, respiratory features and fever are seen in >80% of patients, with lymphadenopathy and/or skin lesions in 50-60% of patients. Anaemia, hepatosplenomegaly and weight loss are also relatively common. Bone lesions are seen in about 25% of patients. Adult-onset immunodeficiency syndrome (with anti–IFN-γ autoantibodies) is very common in this group. |
| FREQUENCY AND GLOBAL BURDEN All cases originate from southeast Asia, notably Thailand, Vietnam, Hong Kong, southern China, Taiwan, India, Indonesia, Cambodia and Laos, unless laboratory acquired. 10% of AIDS patients in Hong Kong and ~30% of patients in N. Thailand present with a T. marneffei infections. Patient with AIDS and penicilliosis present all over the world, following travel. |
| RISK FACTORS Late HIV infection with CD4+ counts less than 100 x106/L. Adult-onset immunodeficiency syndrome. Uncommonly other immunocompromised patients and other patient groups such as those with diabetes, prior tuberculosis, chronic hepatitis and others. |
| DIAGNOSIS In disseminated disease, bone marrow culture gives the highest yield (~100%), followed by skin biopsy (90%) and blood culture (76%). On gram stain of a positive blood culture, septated hyphae-like structures are seen, despite T. marneffei existing in yeast form at 37°C. These hyphae break down into arthroconidia-like yeast cells over time. Over 80% of patients with disseminated penicilliosis are galactomannan antigen (‘Aspergillus’) positive in sera. In high grade fungaemia, intracellular yeast cells may be seen within monocytes on a peripheral blood smear. Fine-needle aspiration of lymph nodes, sputum cytology and touch smear of skin may show small yeasts within histiocytes or extracellularly. Tissue reaction is often muted. T. marneffei may be confused with H. capsulatum but has a central transverse septum unlike any other common pathogenic yeast. In those with only pulmonary disease, fungal culture of bronchoalveolar lavage fluid will yield the organism – there are few data on galactomannan testing. A new antigen Mp1p has shown excellent utility as a novel diagnostics and is in commercial development. |
| TREATMENT The mortality of untreated T. marneffei infection is 100%. Treatment of choice is amphotericin B (0.7-1.0mg/kg) for 2 weeks followed by oral itraconazole 400mg per day for 10 weeks. Itraconazole treatment alone is effective but has a higher 24-week mortality if used as primary therapy, and a higher relapse and immune restoration inflammatory syndrome (IRIS) rate. Simultaneous initiation of anti-retroviral treatment with amphotericin B or at the start of itraconazole therapy is appropriate. IRIS is rarely reported in patients with penicilliosis. Anti-retroviral treatment should not be withheld because of concern for possible development of IRIS. Secondary prophylaxis with itraconazole 200mg/day is highly effective in reducing relapse. |
| OUTLOOK If the diagnosis is made promptly, and initiation of antifungal therapy given, the outlook is good. Central nervous system involvement is more difficult to treat, with a poor outlook. |

Images
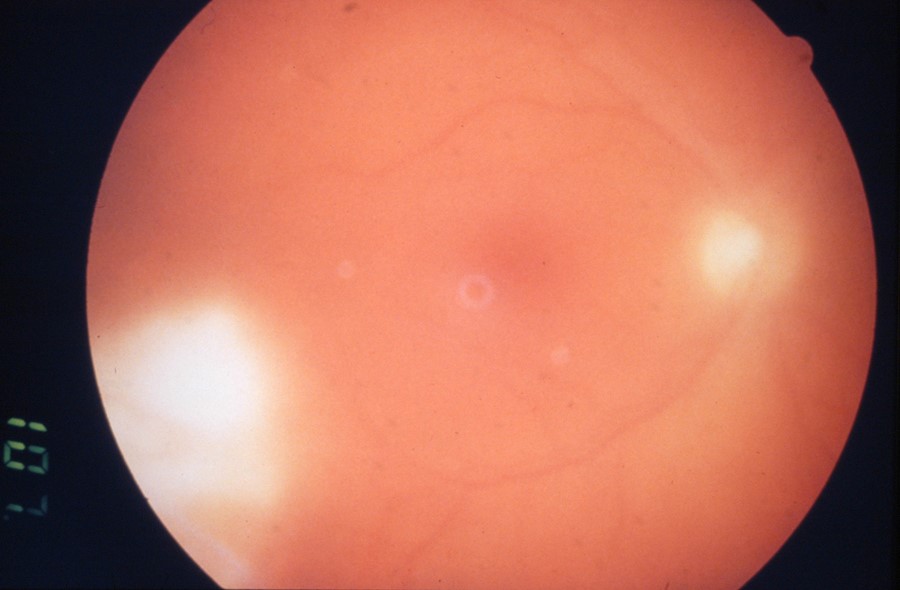
T. marneffei endophthalmitis as a part of disseminated infection in AIDS. 
Molluscum contagiosum-like lesions on the forehead from a laboratory acquired case of T. marneffei infection in context of unsuspected HIV infection. 
Small skin lesions with septic appearance, a manifestation of disseminated T. marneffei infection in AIDS, acquired in Thailand, presenting in the UK. 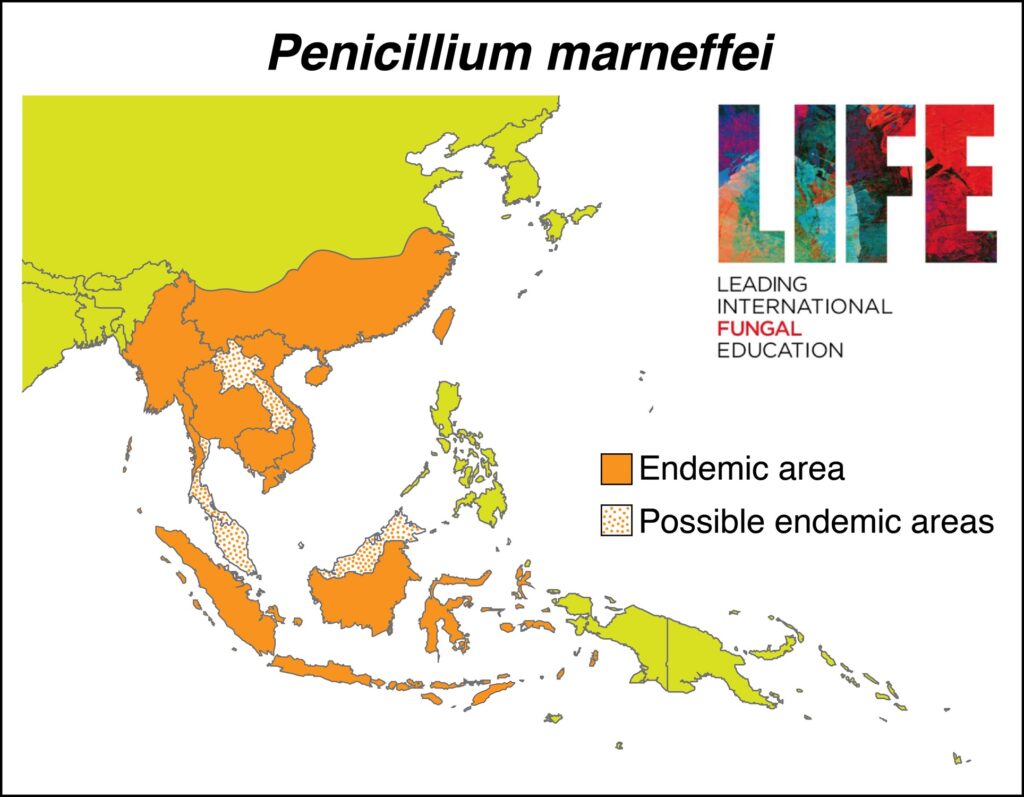
Geographical location of T. marneffei infection in SE Asia
