Factsheets
Invasive aspergillosis
| NAMES Invasive aspergillosis (IA), invasive pulmonary aspergillosis (IPA) For more information please visit the Aspergillus & Aspergillosis Website |
| DISEASE Life-threatening; usually silent disease in its early stages. |
| FUNGI A. fumigatus, A. flavus, A. terreus, A. niger, A. nidulans. Occasionally other Aspergillus spp. |
| GLOBAL BURDEN Over 30 million people are at risk each year because of corticosteroid or other therapies, and over 300,000 patients develop it annually. Worldwide, at least 125,000 of these cases are in COPD. |
| RISK FACTORS It is common in people with acute leukaemia, HSCT and solid organ transplants (especially lung). Less commonly, invasive aspergillosis occurs in people with COPD, medical intensive care, autoimmune disorders (such as SLE), liver cirrhosis, severe burns. However, as some of these diseases are more prevalent than haematological cancer and transplanted patients, the number of individuals with invasive aspergillosis is much higher. Invasive aspergillosis complicates severe influenza (8-24%) and severe COVID-19 (~13%). |
| DIAGNOSIS The key tests are CT scans, biopsy for histology (if possible), Aspergillus antigen test and/or PCR on blood (leukaemia or HSCT) or sputum/BAL. Microscopy for hyphae and culture are insensitive and slow No single test can confirm the diagnosis of invasive aspergillosis, and different tests perform differently in different patient groups. Point-of-care tests for antigens are now available. In intensive care, microscopy, culture and preferably antigen testing of bronchoscopy or tracheal fluids are critical for diagnosis. |
| TREATMENT Voriconazole is the most effective agent, with alternatives including amphotericin B (liposomal or lipid formulations), micafungin, caspofungin, posaconazole or itraconazole. Flucytosine has a limited role. Current guidelines |
| OUTLOOK Early diagnosis and prompt treatment is often successful but unfortunately the diagnosis is frequently made late and patients may die. The status of the underlying disease is important in recovery, as continuing immunodeficiency is problematic. Without treatment the mortality rate exceeds 99%. The best outcomes are in leukaemia patients (30%), but outcomes are worse in other blood malignancies and immunodeficiencies. |
| COVID-19 The overall COVID-19-associated pulmonary aspergillosis (CAPA) incidence is 13% and tends to be in those requiring invasive mechanical ventilation. The time to CAPA diagnosis from illness onset varies between 8 and 16 days. Most patients (>75%) had positive lower respiratory tract cultures for Aspergillus. BAL galactomannan was positive in ~45% and serum in ~18% of patients. The overall mortality of CAPA is >50%, and 2.8 times that of COVID-19 alone. See Chong & Neu, 2021 and Singh et al, 2021. |

Aspergillus infection of bone in the foot in someone with the rare inherited immunodeficiency disorder chronic granulomatous disease 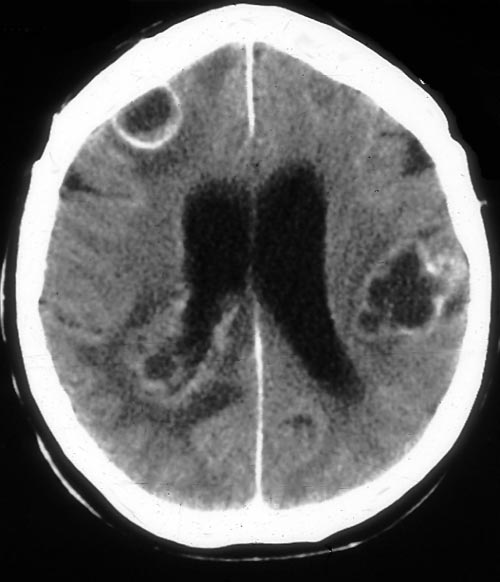
Abscesses in the brain caused by Aspergillus spp. known as cerebral aspergillosis. This is also a feature of disseminated aspergillosis, and is often fatal 
Aspergillus endophthalmitis (infection of the retina of the eye), following dissemination from the lung 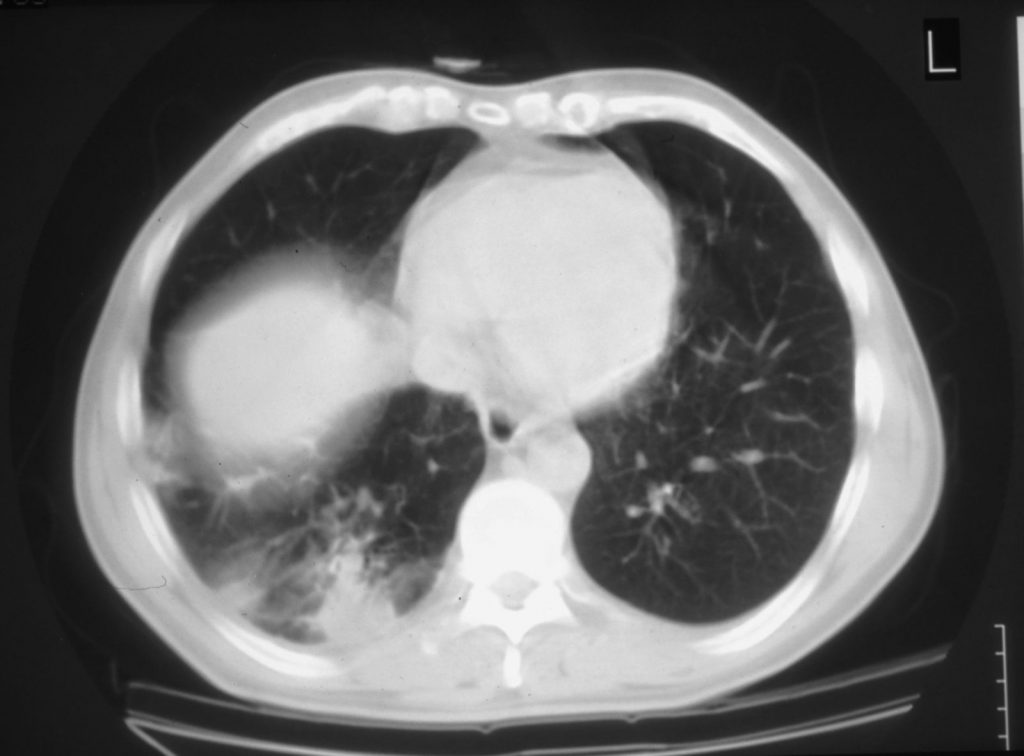
CT scan of the chest. Invasive aspergillosis in AIDS caused by A. niger showing diffuse consolidation at the right base, invisible on the chest radiograph 
CT scan of the chest. Circular cavity in the left lung containing some dead lung invaded with Aspergillus, a feature of healing invasive aspergillosis after recovery of white cells in a patient with leukaemia 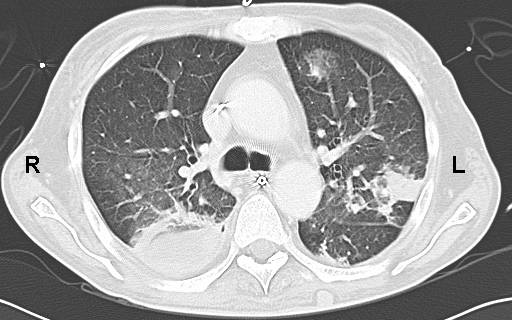
CT scan of the chest. Invasive aspergillosis in leukaemia showing bilateral shadows, a feature of severe disease. On the left is a box-like shadow with some areas of grey surrounding it, known as ground glass (or halo sign). This is more obvious anteriorly

Mucormycosis
| NAMES Invasive mucormycosis, zygomycosis |
| DISEASE Mucormycosis is always life-threatening and invasive. Without treatment mortality is nearly 100%. The clinical presentation is similar to invasive aspergillosis with little fever and few clinical features. Clues to the diagnosis of mucormycosis include progression of the disease on voriconazole or echinocandin therapy, high white blood cell count and elevated inflammatory markers, palatal ulcer with eschar, pulmonary nodules, consolidation or cavitation with negative Aspergillus antigen (galactomannan), Aspergillus PCR and/or beta-D-glucan. Sometimes haemoptysis is the presenting feature. Isolated renal mucormycosis presents abruptly with fever, loin pain, oliguria/anuria and haematuria, in previously well people. Common patterns: – Invasive (fulminant rhino-orbito-cerebral mucormycosis (as it involves nose, eye and brain) – especially in poorly controlled diabetes and haematological malignancy – Pulmonary mucormycosis– especially in haematological malignancy and transplant patients and related to desferrioxamine (deferoxamine) therapy with renal impairment – Cutaneous and wound mucormycosis – especially in burn wound, contaminated traumatic injury, including tsunami and tornado-type events. Increasingly healthcare-related cutaneous mucormycosis are reported. Less common manifestations: – Disseminated mucormycosis – GI mucormycosis – Isolated renal mucormycosis – in SE Asia – Cerebral mucormycosis – especially IV drug users – Foci of disease following disseminated mucormycosis in different organs including heart and liver especially. |
| FUNGI Many fungi in the order Mucorales cause mucormycosis, including Rhizopus oryzae (most common), Rhizopus microsporus, Lichtheimia corymbifera, Lichtheimia ramosa, Rhizomucor pusillus, Mucor circinelloides, Apophysomyces elegans, Cunninghamella bertholletiae, Saksenaea vasiformis |
| GLOBAL BURDEN Up to 11% of filamentous fungal infections in leukaemia are mucormycosis (~5,000 cases annually). In large series of patients with mucormycosis, about 15% of cases were related to malignancy and bone marrow transplantation, implying around 35,000 cases annually worldwide, probably a significant underestimate because of the difficulties in diagnosis. In 16-23% of patients, mucormycosis was reported as diabetes-defining illness. Incidence of the cutaneous form is hard to estimate but seems to have increased in recent years (Skiada et al, 2012). Mucormycosis is much more common in India than most other countries, 14/100,000 (Prakash, 2019), and 10,000s of cases have followed the COVID-19 pandemic there. |
| RISK FACTORS Multiple risk factors may be seen in the same patient. Though similar risk factors are also seen in other invasive fungal infections, metabolic acidosis, and iron overload strikes out in mucormycosis – Immunosuppression, especially haematological malignancy and transplantation – Poorly controlled diabetes – High dose corticosteroids – Desferrioxamine (for iron overload) – Malnutrition and prematurity – IV drug abuse – Contaminated wounds/dressings – Contaminated hospital air Tacrolimus (an anti-rejection agent) appears to be protective against mucormycosis. Mucormycosis can complicate treatment of COVID-19, especially in diabetic patients and/or those given corticosteroids, and may present even after COVID-19 has resolved. See Agrawal et al, 2020 for more information on risk factors. |
| DIAGNOSIS For pulmonary mucormycosis, a ‘reverse halo’ sign can be an early radiological feature. Most diagnoses are made by direct microscopy and histology on a biopsy or sample collected from deep tissue. This is because there are no antigen tests or commercial PCR, and culture is positive in ~10% of cases only. Sometimes microscopy of respiratory fluids or surface swabs will reveal characteristic non-septate branching hyaline (not coloured) hyphae. In most cases, there are many fungal hyphae present, but being confident that they are not Aspergillus or another filamentous fungus, requires experience and sufficient material. The individual fungi responsible can be identified using molecular tools or microscopy. Susceptibility testing is difficult and not validated for these fungi. |
| TREATMENT Surgical debridement or resection is critical, and antifungal therapy is secondary and moderately effective. Amphotericin B and posaconazole are the only active antifungal agents. Reversal of the underlying disease is also and important step Current guidelines |
| OUTLOOK Approximately 70% of patients survive mucormycosis in the short term. Disseminated disease, bilateral pulmonary infection, cerebral infection, burn wound, uncontrolled malignancy and severe malnutrition are all poor prognostic features. |

Pulmonary mucormycosis in a patient with acute leukaemia 
Pulmonary mucormycosis in a patient with acute myeloid leukemia given voriconazole prophylaxis to prevent fungal infection. This was surgically removed and she went to complete her chemotherapy successfully 
Cutaneous mucormycosis 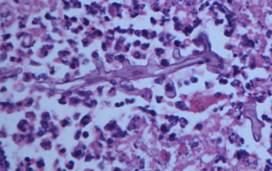
Cutaneous mucormycosis 
Cutaneous mucormycosis 
Macroscopic photograph shows Mucor sporangia growing on old bread.