Fungi can infect various parts of the eye but the most common infections are fungal keratitis, Aspergillus endophthalmitis and Candida endophthalmitis.
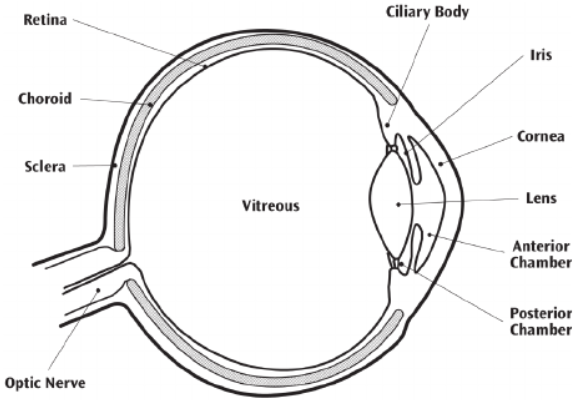

Factsheets
Fungal keratitis
| OVERVIEW Fungal keratitis can follow ocular injury (~50%) or contaminated contacts lens fluid, invasion of the transparent cornea by fungi leads to inflammation and loss of vision. Symptoms as in any other type of keratitis, but, perhaps, more prolonged in duration (5-10 days). For reviews, see Thomas & Kaliamurthy (2013) or Badiee (2013) |
| FUNGI Aspergillus flavus, Aspergillus fumigatus, occasionally other Aspergillus spp. Fusarium spp. Candida albicans. Less commonly Curvularia lunata, Scedosporium apiospermum, Bipolaris spp., Lasiodiplodia theobromae, Cephaliophora irregularis, Colletotrichum dematium and others. |
| GLOBAL BURDEN There are estimated to be over a million cases of fungal keratitis annually worldwide most in tropical countries. Bacterial keratitis is more common in contact lens wearers and the western world, whereas in India and Nepal and some other countries, fungal keratitis is at least as common as bacterial keratitis. |
| RISK FACTORS Trauma especially if associated with plant material is a common antecedent to fungal keratitis. Contact lens fluid contaminated with fungi (e.g. Fusarium) may lead to a mini-outbreak of fungal keratitis. Other possible risk factors include topical corticosteroids, traditional medicines and higher external temperatures and humidity. |
| DIAGNOSIS SPECIMEN: material from the affected part of the cornea, collected by scraping any area of ulceration, or biopsy when the corneal epithelium is intact and the infection is within the corneal stroma. How to take a corneal scrape: Leck (2015) COLLECTION: (see Leck, 2015) Material should be collected from the base and edges of the ulcerated part of the cornea. Calcium alginate swabs pre-moistened with tryptone soya broth used for debridement may facilitate recovery of fungi in culture. TESTS: Microscopy (lactophenol cotton blue, gram stain and Calcofluor white) and culture (and possibly PCR) are necessary, because of the wide variety of fungi involved. Prolonged culture (3 weeks) at 25ºC or 30ºC may be necessary. |
| TREATMENT For a review, see Upadhyaya et al (2009) Topical antifungal therapy is essential, with the severity of the disease dictating how frequently eye drops are administered. In severe cases this is hourly, and can be reduced in frequency after 1- days as improvement is documented. SUPERFICIAL LESIONS: caused by filamentous fungi, topical natamycin 5%, amphotericin B 0.15% or voriconazole 2-3% (50 µg/ml) are usually used. For Candida, amphotericin B 0.15% or voriconazole 2-3% may be used. SEVERE INFECTIONS: oral therapy is also advised: voriconazole, fluconazole (if Candida) or itraconazole (if Aspergillus). Alternative therapies include topical (1%) and subconjunctival (10 mg) miconazole or topical itraconazole suspension (1%). Therapy is usually continued for at least 14 days. Surgical debridement is essential for severe disease (link to section under surgery). |
| OUTLOOK Fungal keratitis is associated with a ~5- fold higher risk of subsequent perforation and need for penetrating keratoplasty than bacterial keratitis. Recovery of sight is higher if the diagnosis is made early. Topical antifungal therapy has a 60% response rate with retention of vision if keratitis is severe and a 75% response if milder. |
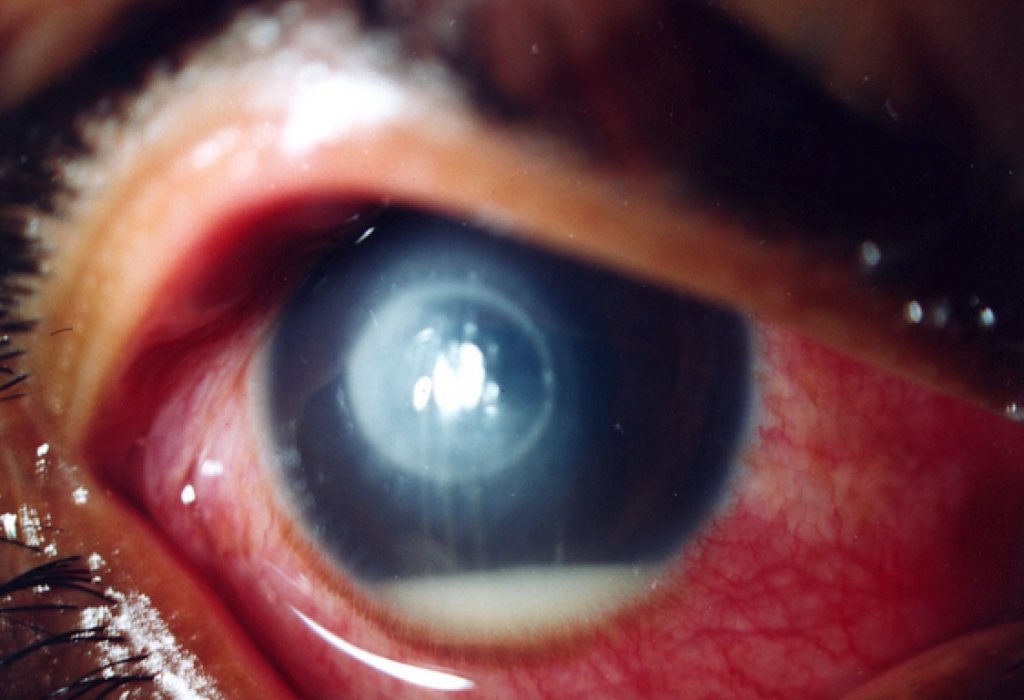
Severe fungal keratitis (Dr Philip Thomas) 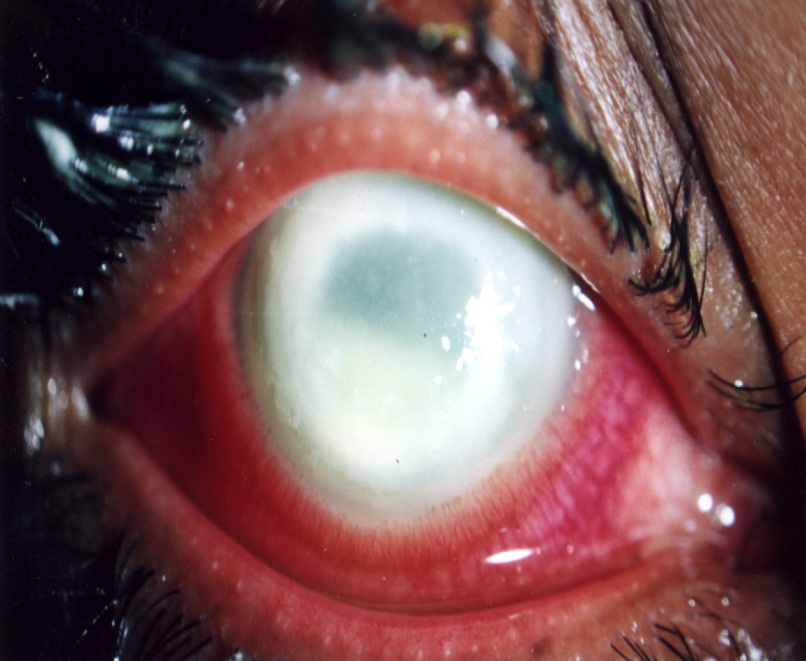
Complete corneal opacifiaction following fungal keratitis, which is only remediable with a corneal transplant.

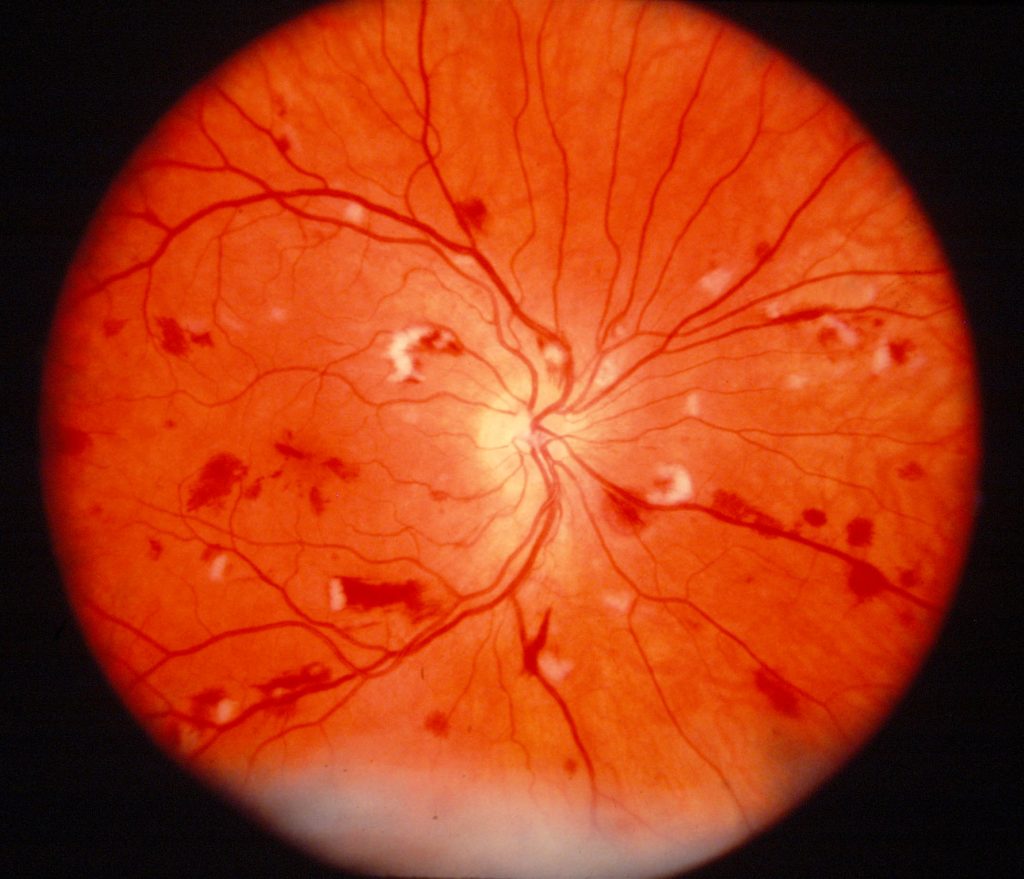
Candida endophthalmitis
| OVERVIEW Candida endophthalmitis retinal lesons may take 14 days to evolve and by the time symptoms are apparent, many patients will have progressed to multiple bilateral lesions. – For detailed clinical recommendations, please refer to the IDSA guidelines (Pappas et al, 2016). – For a detailed discussion of the use of different antifungals and their formulations, please see Khan et al (2007). |
| FUNGI Primarily Candida albicans. Occasionally C. krusei or C. glabrata. Sometimes C. tropicalis in neonates (Baley & Ellis, 2003). |
| GLOBAL BURDEN The rate of developing candida endophthalmitis in the setting of candidemia has ranged from 28–45% in different reports. |
| RISK FACTORS Eye surgery/trauma. Candidaemia. Immunosuppression, CVC, diabetes mellitus, intravenous drug use. |
| DIAGNOSIS IDSA guidelines (Pappas et al, 2016) recommend that candidaemia patients should receive a dilated retinal examination carried out by an ophthalmologist. Ultrasound examination is mandatory in case of suspected endophthalmitis (Spadea & Giannico, 2019). Vitreous and aqueous samples may be collected during pars plana vitrectomy (Celiker & Kazokoglu, 2020). |
| TREATMENT Intravitreal injection of amphotericin B or voriconazole (Bienvenu et al, 2019), and/or vitrectomy. |
| OUTLOOK Poor – loss of sight is common. Candida endophthalmitis in critically ill patients is a strong predictor of mortality (up to 80%). |

Aspergillus endophthalmitis
| OVERVIEW Aspergillus enters the intraocular fluid either following trauma/surgery, or endogenously from the bloodstream. Aspergillus and Fusarium endophthalmitis are often associated with long-term corticosteroid treatment or intravenous drug use. It can also occur as a consequence of fungal keratitis. – For reviews, see Spadea & Giannico (2019) or Dave et al (2020) – Read a clinical guide to diagnosis and treatment of endophthalmitis at EyeWiki |
| FUNGI Most commonly Aspergillus fumigatus and A. flavus. Less frequently A. niger, A. terreus, A. ustus, A. glaucus, A. versicolor, A. conicus. Fusarium is another common genus of mould associated with fungal endophthalmitis. |
| GLOBAL BURDEN “The incidence of endophthalmitis ranges from 0.03-1.3% following cataract surgery and can be as high as 30-40% following open globe injuries. Fungal endophthalmitis accounts for 8.6-18.6% of culture-positive cases” (Spadea & Giannico (2019) |
| RISK FACTORS – Exogenous: cataract surgery, trauma – Endogenous: immunosuppression |
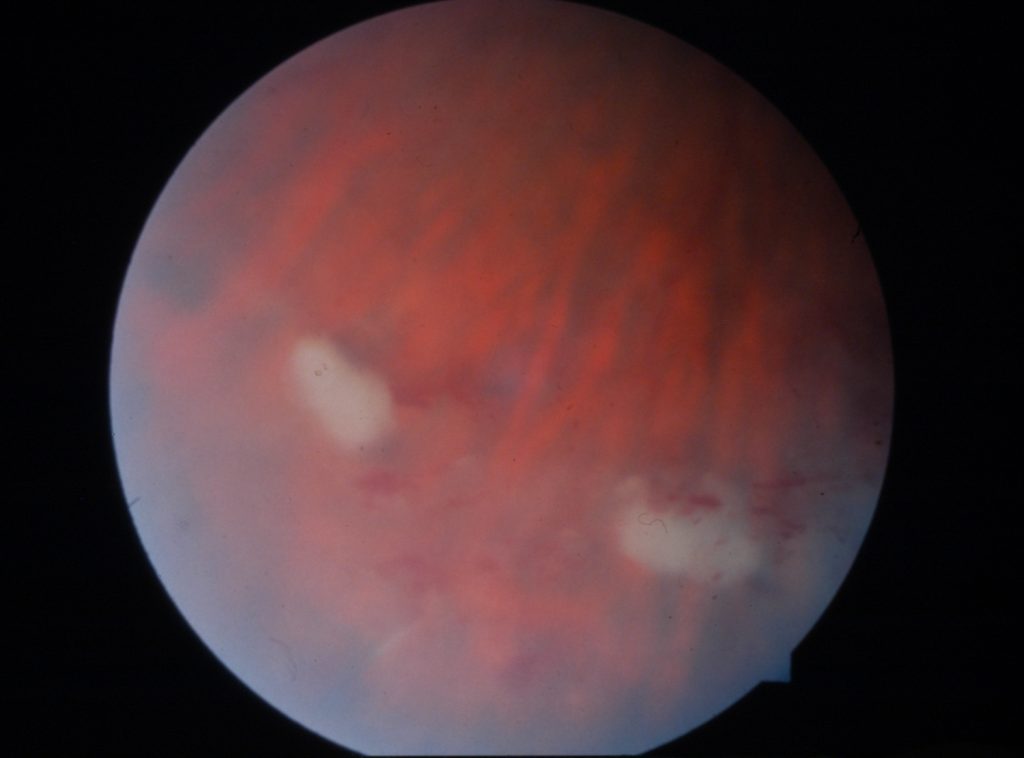
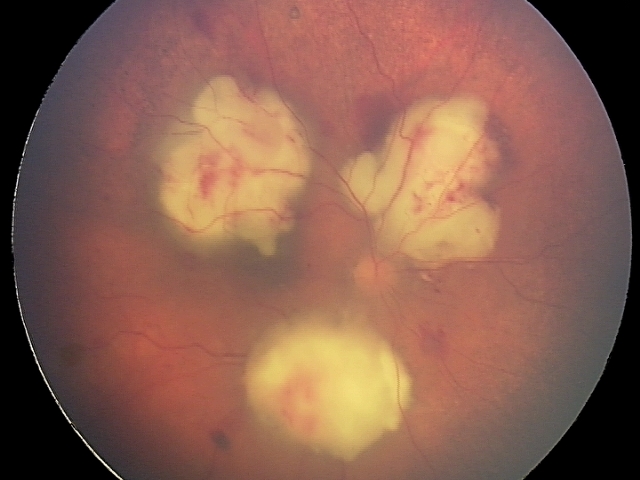
| DIAGNOSIS Fundus examination may show white retinal lesions, or even detached retina. Ultrasound examination is required is the fundus cannot be adequately visualised with retinography (Spadea & Giannico, 2019). Vitreous and aqueous samples may be collected during pars plana vitrectomy (Celiker & Kazokoglu, 2020). Culture on Sabouraud, or carry out PCR/FISH if available. |
| TREATMENT Intravitreal amphotericin B (5 mg/0.1 ml) or voriconazole (up to 100 microgram/ml) is safe for the retina. Alternatively systemic voriconazole or caspofungin for at least 1 month. Combinations may also be effective (e.g. Mithal et al, 2015) If severe inflammation is present, steroids may be used with care. |
| OUTLOOK Prognosis often poor, especially when diagnosis is delayed. Enucleation and loss of vision are not uncommon. – For more information on prognoses see Dave et al (2020) |
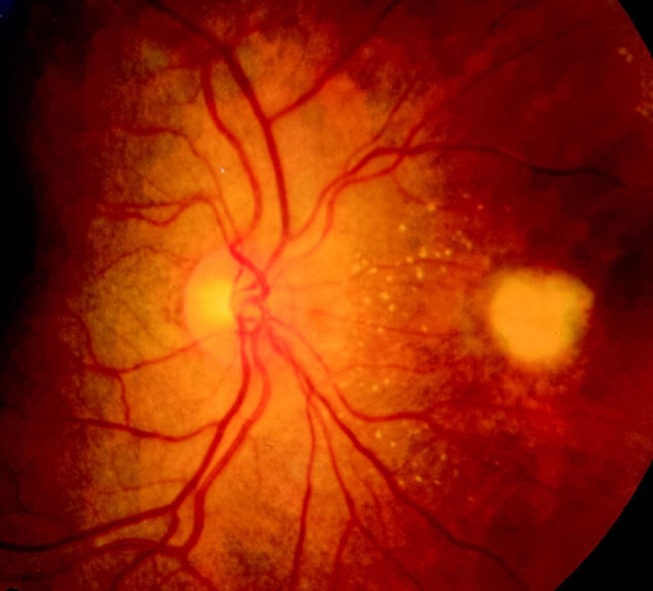
Fundus examination shows white retinal lesions caused by Aspergillus. From Spadea & Giannico (2019) 

Other fungi causing endophthalmitis
Cryptococcal endophthalmitis 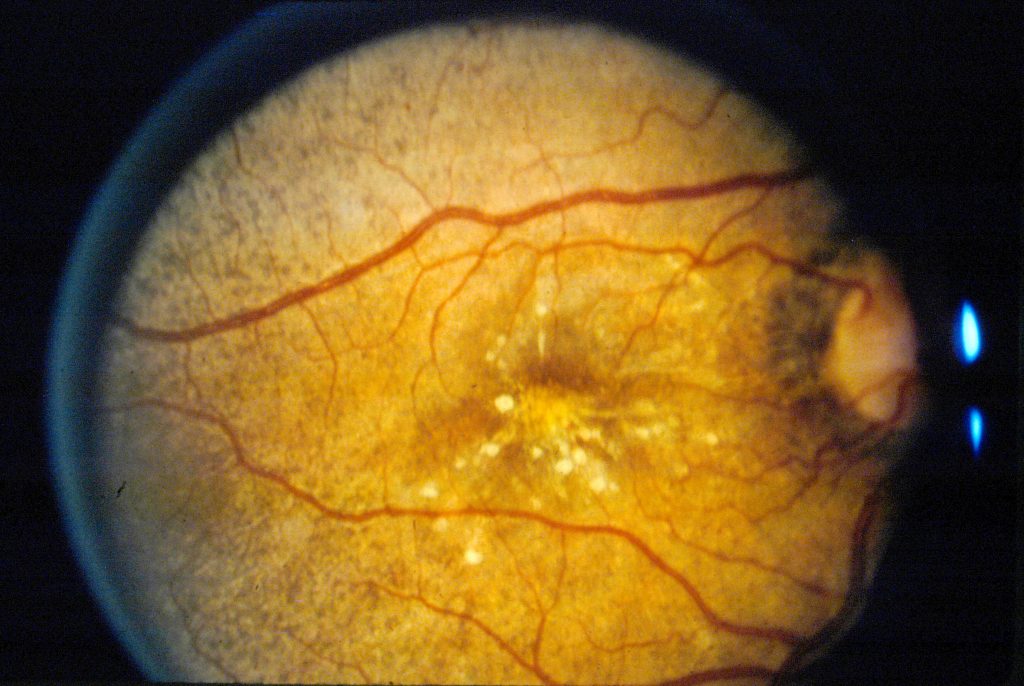
Coccidioides endophthalmitis – note spherical lesions near macula

