Antifungal resistance is gradually rising. The reasons are multiple, including:
- Emergence of new, resistant species such as Candida auris and Trichophyton indotineae
- Replacement of susceptible species with resistant ones in patients on antifungal prophylaxis or therapy (ie Candida glabrata on fluconazole)
- Emergence of resistance on therapy (ie Aspergillus fumigatus treated with itraconazole or voriconazole or Cryptococcus neoformans treated with fluconazole)
- Emergence of azole resistant Aspergilli from the agricultural use of azole fungicides.
Some species of fungi are intrinsically resistant to certain or multiple antifungals. Commoner examples are Candida krusei and to fluconazole, Aspergillus terreus to amphotericin B, Aspergillus calidoustus to azoles, Fusarium spp. to fluconazole and Mucorales to voriconazole. In these cases, species identification is sufficient, and for the known resistance pattern, actually doing a susceptibility test to that antifungal is unnecessary (although sometimes done as part of a panel).
The vast majority of fungal susceptibility tests are done on positive cultures. In recent years, direct molecular (PCR) detection of some resistant markers have been commercially introduced.

Culture-based susceptibility testing
Reference systems for antifungal susceptibility testing
Academic efforts in the US (NCCLS, now CLSI) and in Europe (EUCAST) from the mid 1990’s lead to defined methods for identifying antifungal resistance, initially in common Candida species against fluconazole and Aspergillus spp. against itraconazole. These methods evolved over many years to embrace additional antifungals and fungi.
EUCAST AFST Committee provides a comprehensive reference method for antifungal susceptibility testing of Candida spp., Cryptococcus spp., Aspergillus spp., and more recently dermatophytes. The method is in microtitre plates, using RPMI with glucose medium and requires careful inoculum preparation, and care in endpoint reading. Yeast and dermatophyte MICs are read with a spectrophotometer, Aspergillus spp. by eye. Detailed methods are here: www.eucast.org/astoffungi/methodsinantifungalsusceptibilitytesting
Interpretation and reporting guidance is here: www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/AFST/Clinical_breakpoints/AFST_BP_v10.0_200204_updatd_links_200924.pdf
Clinical and Laboratory Standards Institute (CLSI) provides alternative microtitre methods for susceptibility testing of Candida spp., other yeasts and filamentous fungi, including Aspergillus spp. It utilises round bottom microtitre plates and visual endpoint reading. An earlier full version of the method for yeasts is here:
https://clsi.org/media/1461/m27a3_sample.pdf
The up-to-date 2022 version is here: https://clsi.org/standards/products/microbiology/documents/m27m44s/
An older version of the method for filamentous fungi is here: https://clsi.org/media/3682/m61ed2_sample.pdf and the up to date (2022) version is here: https://clsi.org/standards/products/microbiology/documents/m38m51s/
Interpretation guidance based on epidemiological cut-off values is here:
https://clsi.org/standards/products/microbiology/documents/m57s/
These systems have been used for defining resistance breakpoints, if possible based on correlative therapeutic outcome data. If not possible, because of data limitations, the alternative approach to defining resistance is based on epidemiological cut-off values (ECV) (ie outliers). Almost all endpoints describe inhibition; older assays also described fungicidal concentration, but these are much less frequently used in clinical practice.

Commercial systems for antifungal susceptibility testing
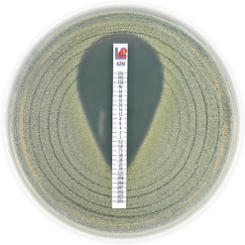
Several commercially available systems are available as part of complete solutions for laboratories including disks for disk diffusion assays and pre-filled microtitre plates for microbroth dilution testing. Some complete systems include eTest and several microtitre systems, some with colour change reagents to aid endpoint reading. Other systems integrate yeast identification with susceptibility testing.
Diffussion gradient strips:
BioMerieux www.biomerieux-diagnostics.com/etestr

Lilofilchem www.liofilchem.com/solutions/clinical/arm/mts-mic-test-strip
Vitek link: www.biomerieux-diagnostics.com/vitekr-2-0

Sensititre microtitre links: https://www.thermofisher.com/order/catalog/product/YO9

Premade susceptibility microtitre plates for EUCAST Merlin Micronaut: https://www.merlin-diagnostika.de/en/products/susceptibility-testing-ast/index.html

Candida and other ascomycete yeasts
Candida spp. recovered from blood cultures or other deep tissue (normally sterile) samples should be tested for antifungal susceptibility as acquired resistance to azoles and echinocandins is an increasing concern. CLSI or EUCAST microbroth dilution protocols are the standard procedures. Commercial microbroth dilution kits (e.g. Sensititre YeastOneTM) or diffusion gradient (commonly known as Etests) are acceptable alternatives. Mass spectrometry can also provide susceptibility results and one such system is the Vitek 2. Clinical breakpoints (CBP) to define susceptibility or resistance have been assessed by EUCAST and CLSI for the most relevant pathogenic Candida spp. Among normally susceptible Candida spp. (e.g. C. albicans), fluconazole resistance is observed at variable frequency depending on the epidemiological context (only 2-5% in USA and Europe). C. glabrata is usually considered as ‘susceptible dose-dependent’ and exhibits variable susceptibility to azoles. C. krusei is intrinsically resistant to fluconazole, but not to voriconazole. For C. auris, there is no established CBP, but tentative breakpoints have been proposed by the Centers for Disease Control and Prevention (CDC, available at: www.cdc.gov/fungal/candida-auris/c-auris-antifungal.html). More than 90% of C. auris isolates have acquired resistance to fluconazole. Echinocandin resistance is rare (<5%) but is a growing concern among C. glabrata and C. auris because of their frequent association with azole resistance and the emergence of multi-resistant isolates for which therapeutic options are limited.
Relevant links:
https://www.cdc.gov/fungal/lab-professionals/pdf/afst-yeasts-h.pdf
https://www.biomerieux-usa.com/clinical/etest

Conidia-forming moulds (filamentous fungi)
Antifungal susceptibility testing is recommended for Aspergillus spp. (in particular A.fumigatus) when isolated from clinically relevant samples because of the emergence of acquired azole resistance. Testing should be performed by CLSI or EUCAST microbroth dilution protocols. Commercial microbroth dilution kits (e.g. Sensititre YeastOneTM) is an acceptable alternative. Etests can be performed but may provide significantly lower values for posaconazole. Clinical breakpoints (CBP) have been proposed by EUCAST for some Aspergillus spp. and antifungal drugs (azoles, amphotericin B), but not CLSI.
Antifungal susceptibility testing is not routinely recommended for non-Aspergillus pathogenic moulds (e.g. Mucorales, Fusarium, Scedosporium) because of the lack of correlation between MIC and outcomes and the absence of interpretive clinical breakpoints. However, it can be performed on a case by case evaluation to help for therapeutic decisions.
Cryptococcus spp.
Many centres undertake susceptibility testing of Cryptococcus spp. While there are some resistant isolates, and rising MICs during therapy in some patients, the breakpoint for resistance and the correlation of MIC with clinical or experimental model therapeutic outcome is poor. Gradient diffusion is not suitable for Cryptococcus neoformans.

Molecular identification of resistance markers
In certain fungi, there are a few dominant genetic resistance markers, allowing the direct detection of resistance, even with a negative culture. There are a couple of challenges to this attractive concept. First, some resistant fungi have several mechanisms of resistance, often concurrently, so detection of a resistance marker allows definitive determination of resistance, but a negative assay does not exclude resistance. Second, most antifungal intracellular targets are coded by single copy genes, whereas identification is often based on multi-copy genes (to enhance sensitivity). Low level PCR signals in identification, may translate into a falsely negative resistance assay.
Aspergillus fumigatus
Azole resistance in Aspergillus fumigatus typically result from hotspot mutations in the azole target gene cyp51A. The most frequent ones consist of a tandem repeat in the promoter and one or more point mutations in the gene (TR34/L98H and TR46/Y121F/T289A). Some commercial PCR kits can directly detect these mutations in clinical samples.
https://www.pathonostics.com/product/aspergenius
Trichophyton spp.
Terbinafine resistance is rapidly emerging, notably in the new species T. indotineae. The common resistance mutations in the squalene epoxidase gene can be directly detected by PCR. Several commercial products are available:
www.pathonostics.com/product/dermagenius

https://bakodx.com/services/terbinafine-resistance-pcr-test/#aawp_nl
Pneumocystis jirovecii
Two sulphamethoxazole mutations can be detected using the PneumoGenius assay: www.pathonostics.com/product/pneumogenius