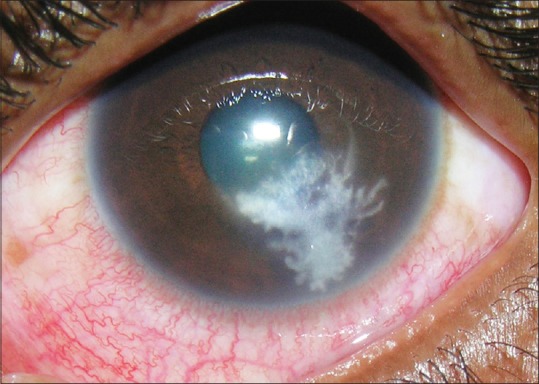
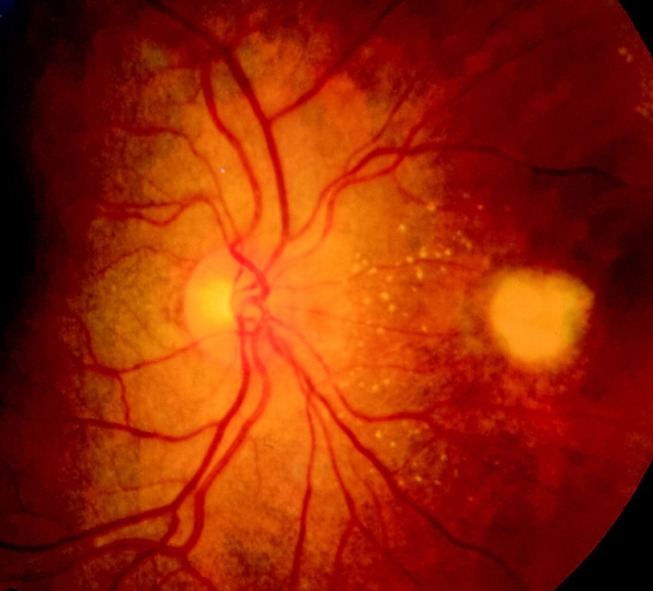
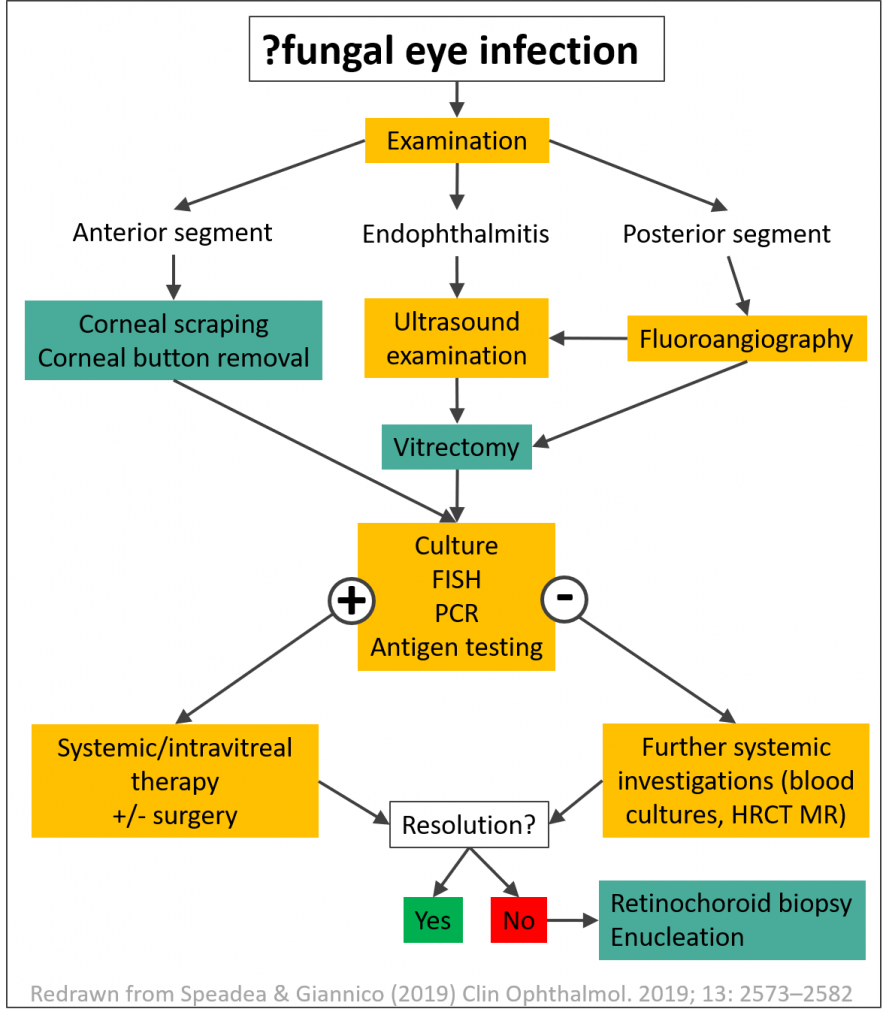
Fungal eye infections are sight-threatening and require immediate specialist (often multi-disciplinary) care. Fungi including Aspergillus, Fusarium and Candida can infect the cornea (keratitis), internal structures (endophthalmitis) and surrounding structures (orbit, conjunctiva, sclera, eyelid, lacrimal apparatus).
- Read our factsheets about fungal keratitis, and Aspergillus or Candida endophthalmitis
- Read reviews about less common fungal eye infections
- Paracoccidioidomycosis (Cataño & Salinas, 2017)
- Visit the Facebook peer support group for presumed ocular histoplasmosis (POHS)
Pathogens can be introduced during trauma or surgery, or spread internally from the bloodstream of immunocompromised patients. Watch for risk factors including: HIV/AIDS, prolonged steroid use, diabetes mellitus, transplant recipients, intravenous drug use and recent cataract surgery.
Many systemic formulations of antifungals have limited penetration into the eyes. Some antifungals can be administered intravitreally, but amphotericin B can cause retinal toxicity at higher doses (Payne et al, 2010). Voriconazole is less toxic but requires more frequent injection(every 24 hours) than amphotericin B (every 48 hours).
Corneal ulcers are a significant public health problem in low-resource settings where many people work in industries (e.g. farming, forestry) with a high risk of traumatic onculation of fungi into the eye, and patients may present later in the course of infection due to poverty. Prajna et al (2017) shared their experiences of carrying out clinical research at Aravind Eye Hospital (India) with these challenges.

Clinical guidelines
- The American Academy of Ophthalmology produces the EyeWiki which gives up-to-date guidance on management of fungal keratitis (and the role of intrastromal injections for fungal keratitis), endophthalmitis, orbital aspergillosis, post-traumatic endophthalmitis, rhino-orbital-cerebral mucormycosis, and other conditions.
- Guidelines for fungal keratitis are also available from WHO (2004, South-East Asia), as well as the Royal College of Ophthalmologists (2013, UK)
- The College of Optometrists (UK) produces Clinical Practice Guidelines for microbial keratitis (2018) and post-operative endophthalmitis (2017).
- IDSA guidelines (Pappas et al, 2016) recommend that candidaemia patients should receive a dilated retinal examination carried out by an ophthalmologist.

Key clinical trials
- MUTT 1 (Prajna et al, 2013) Topical oriconazole (1%) versus natamycin (5%) for filamentous fungal keratitis
- MUTT2 (Prajna et al, 2018) Oral voriconazole versus placebo (in addition to topical antifungals) for fungal keratitis.
- Read more about MUTT1 and MUTT2 at eyewiki.aao.org
- Topical Chlorhexidine 0.2% versus Topical Natamycin 5% for the Treatment of Fungal Keratitis in Nepal (Hoffman et al, 2021)