The detection of fungal pathogens causing respiratory infections is challenging with culture because of low sensitivity, but also the detection threshold of PCR methods. The incorporation of next-generation sequencing (NGS) as a routine diagnostic armamentarium could curb these limitations.
A new study by Yin et al 2024 provides evidence that NGS of bronchoalveolar lavage (BAL) fluid significantly enhances the detection of fungal pathogens compared with conventional microbiology testing (CMT), with detection rates of 56.8%, 73.8%, 76.7%, and 70.5% for CMT, multiplex PCR-based targeted NGS, hybrid capture-based targeted NGS, and metagenomic NGS, respectively.
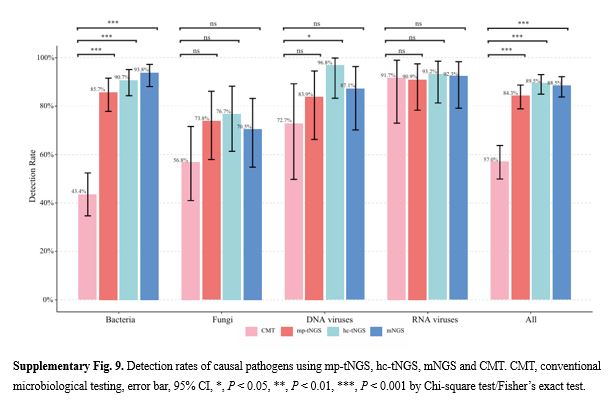
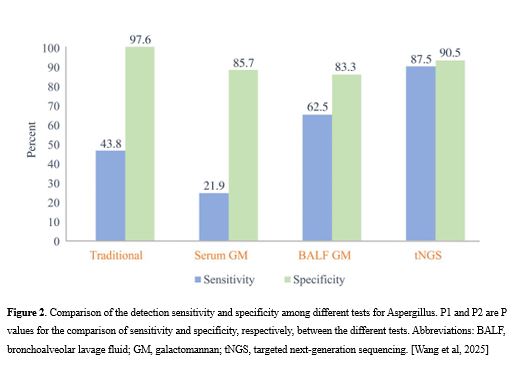
Of particular interest was the significantly higher sensitivity demonstrated by mNGS, mp-tNGS, and hc-tNGS in the detection of Aspergillus fumigatus compared with the galactomannan assay. This suggests that NGS is more effective in cases of probable IPA, where conventional diagnostics often fall short. In addition, the turnaround time for NGS is significantly shorter than that for fungal cultures, offering clinicians a faster path to appropriate treatment. However, there is a need for caution in distinguishing between colonization and IA.
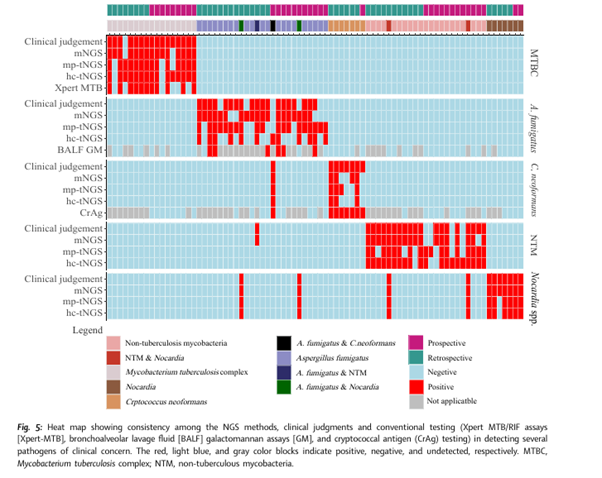
One key advantage of NGS is its ability to identify multiple pathogens in a single test, offering broader diagnostic insight in complex infections. This is particularly useful in immunocompromised or critically ill patients, where coinfections are common.
However, the authors caution that while NGS is a promising tool, its cost, technical requirements, and need for further standardization may limit its immediate adoption in all clinical settings. They advocate for larger, multi-centre studies to validate their findings and explore cost-effectiveness.
This study marks a significant step forward in respiratory infection diagnostics and could pave the way for more personalized and timely antifungal treatment strategies in vulnerable patient populations.
Besides this index study, more studies from China have affirmed the high sensitivity of NGS and its shorter turnaround time compared with CMT [Niu et al, 2024; Wang et al, 2025]