The new Global Guideline for the Diagnosis and Management of Candidiasis (Cornely et al., 2025) is a comprehensive review and update on the diagnosis, treatment, and prevention of Candida infections, developed by the European Confederation for Medical Mycology (ECMM) in collaboration with ISHAM and ASM. Candida species, particularly Candida auris and fluconazole-resistant Candida parapsilosis, pose significant global health threats due to antifungal resistance and increasing incidence in hospitalized patients. The guideline provides updated recommendations for both invasive (e.g., candidemia, deep-seated infections) and mucocutaneous (e.g., oral thrush, vulvovaginal candidiasis) infections.
This new work builds on the previous ESCMID (2012) and IDSA (2016) guidelines.
Epidemiology & Diagnosis
Candida infections occur in immunocompromised and critically ill patients, but mucocutaneous candidiasis can affect healthy individuals. New antifungal-resistant strains, especially C. auris, have become a growing challenge in healthcare settings. Traditional microscopy and culture remain the cornerstone of diagnosis, but molecular methods and biomarker-based diagnostics are evolving. One key recommendation is to collect two to three blood culture sets with each 20 mL blood volume in adults when investigating potential candidaemia. Detailed diagnostic recommendations on endocarditis, Candida CNS infection, ocular candidiasis and chronic disseminated candidiasis are provided in the appendix.
Treatment Guidelines
The guideline strongly recommends echinocandins (e.g., caspofungin, micafungin, anidulafungin) as first-line therapy for invasive candidiasis due to their broad activity and safety. Alternative treatments include liposomal amphotericin B and fluconazole, though resistance is a concern. Rezafungin, a long-acting echinocandin, and ibrexafungerp offer new options for specific infections. Oteseconazole is introduced as a treatment for recurrent vulvovaginal candidiasis.
Invasive candidiasis in special populations (e.g., neonates, transplant recipients) is covered in detail. Prophylactic antifungal therapy is recommended for high-risk groups such as ICU patients and those undergoing organ transplants or chemotherapy.
Infection Prevention & Control
The spread of resistant C. auris necessitates strict infection control measures, including screening high-risk patients, isolation, and environmental decontamination using sporicidal disinfectants like hydrogen peroxide and peracetic acid. The guideline also emphasises antifungal stewardship to ensure appropriate antifungal use and prevent resistance.
Challenges & Future Directions
The emergence of novel antifungals and changing taxonomy present challenges for clinicians. Further research is needed to refine diagnostic approaches, optimise treatment for resistant strains, and evaluate the clinical impact of new antifungal agents.
The supplementary appendix provides detailed methodology, evidence grading, and extensive epidemiological data on risk factors, incidence, and global distribution of Candida infections (and includes 1325 references). It also expands on paediatric candidiasis, species-specific treatment recommendations, and regional adaptations of the guidelines.
This guideline serves as a global reference for managing candidiasis, and shows the need for evidence-based, multidisciplinary care. Although the authors call for standardised recommendations, they acknowledge the need for local adaptations based on resource availability and resistance patterns.
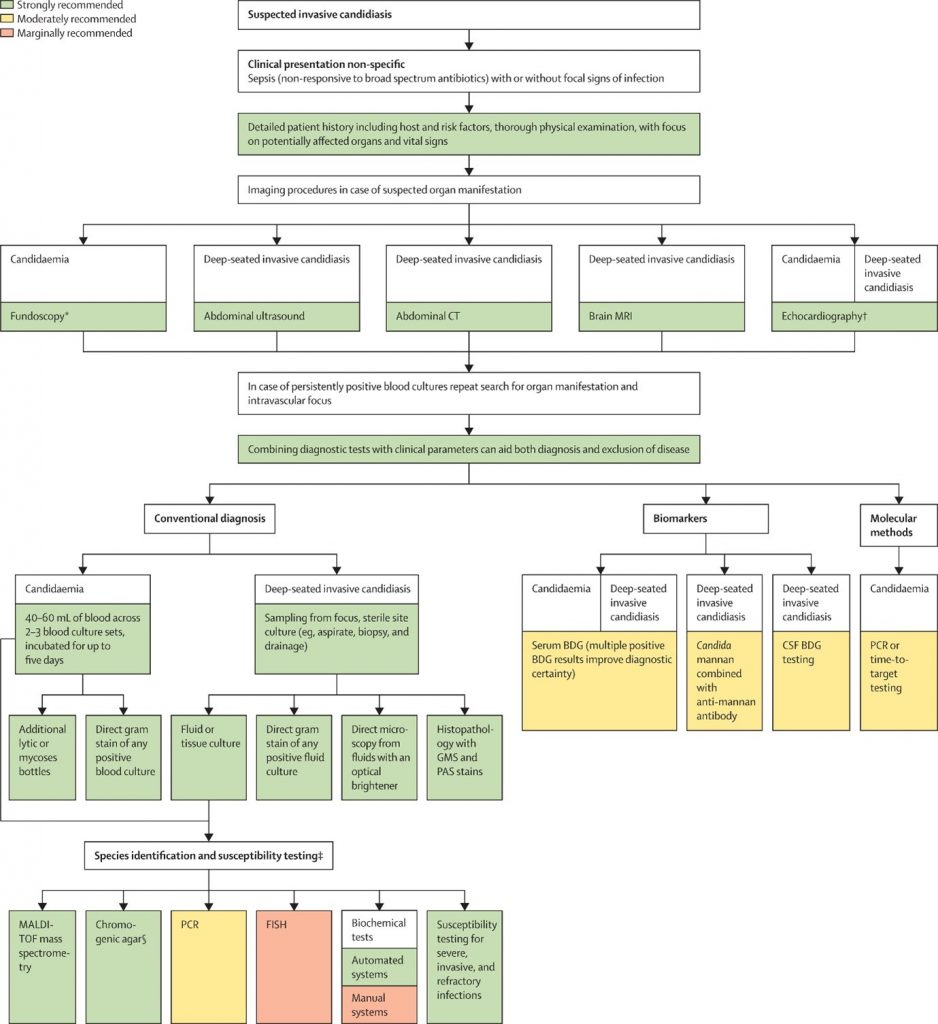
Figure 1 Optimal diagnostic pathway for the diagnosis of candidaemia and invasive candidiasis in adults
