Cryptococcal meningitis is a well-known complication of HIV/AIDS, but less is known about how cryptococcosis presents among patients who are immunosuppressed for other reasons (transplants, autoimmunity, malignancies).
Dr Kieren Marr and colleagues at 20 US centres surveyed 138 immunosuppressed (but HIV-negative) patients with cryptococcosis.
- Around half (49%) of patients had CNS involvement, and a MoCa score <22 was predictive or poor long-term cognitive outcomes.
- Just over a quarter (27.8%) had a fever
- Disease was often diagnosed late (>1 week), especially in those without fever
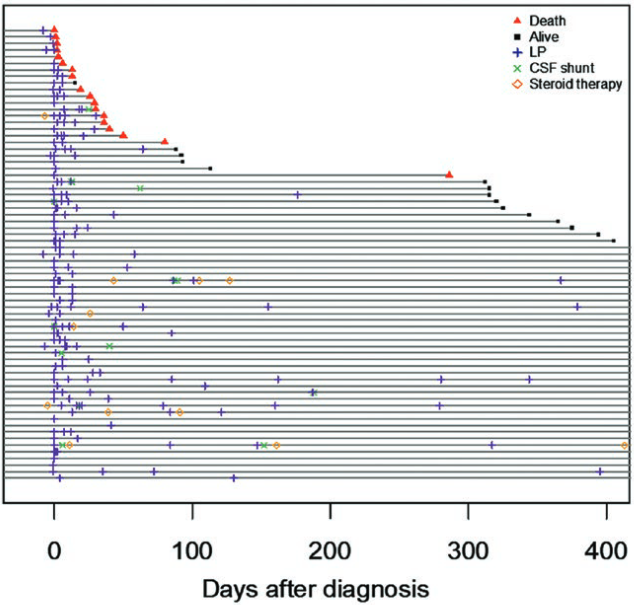
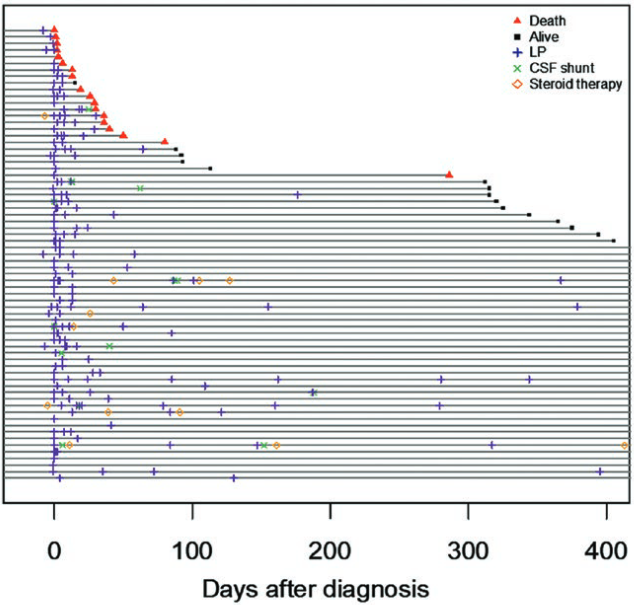
- A dangerous inflammatory response is occasionally seen after resolution of the infection, which is characterised by alternative macrophage activation and paradoxical worsening of the condition as treatment progresses. Ventricular drainage and high-dose corticosteroids can alleviate this
- Five cases were caused by Cryptococcus gattii, with no apparent underlying disease
The number of cases of cryptococcosis in HIV- patients is gradually rising as more people experience complex immunosuppression, for example following transplant or treatment with targeted biological therapies such as anti-TNFα, IL-6 and ibrutinib.
Cryptococcosis in HIV- patients show atypical presentation, leading to delayed diagnosis