Histoplasma capsulatum is an endemic fungus that causes various disease manifestations, including two invasive forms: progressive disseminated histoplasmosis and acute pulmonary histoplasmosis (see factsheets below). It is often mistaken for other conditions including TB and bacterial pneumonia.
While culture from a clinical sample is the current gold standard for diagnosis, antigen testing is useful and can be used to assess response to treatment (Azar & Hage, 2017). A point-of-care test is available from MiraVista for Histoplasma antigen that can be used on serum on urine, which has shown promise in patients groups including those living with HIV/AIDS (Cáceres et al, 2019).

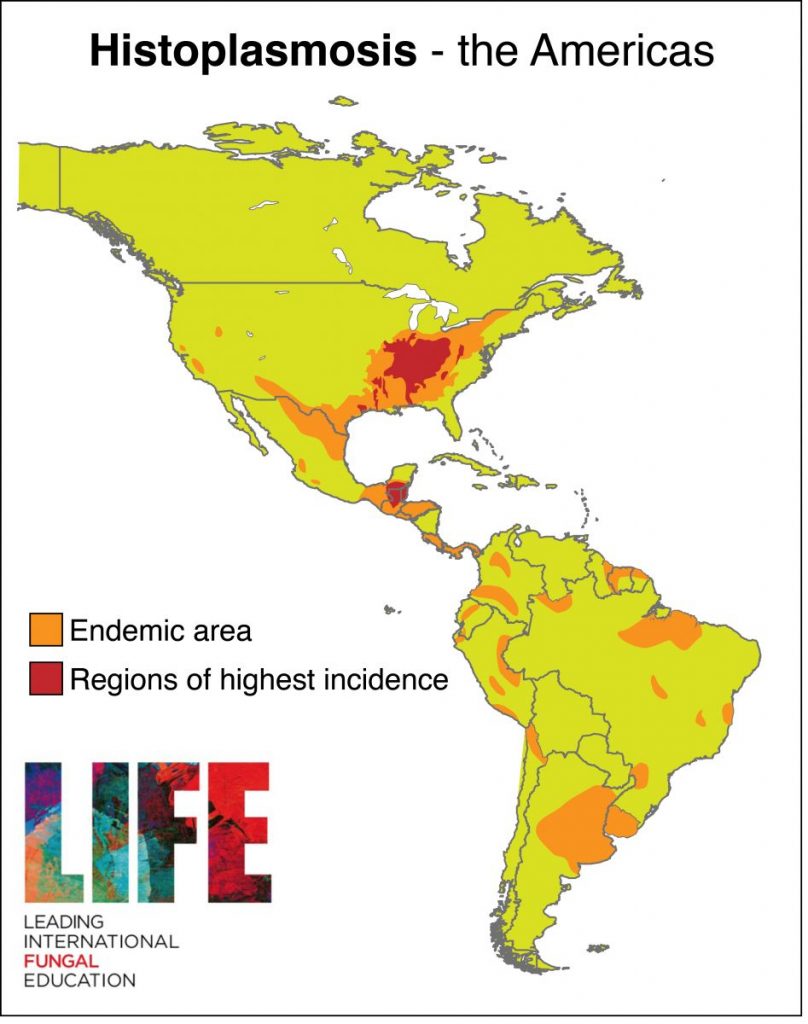
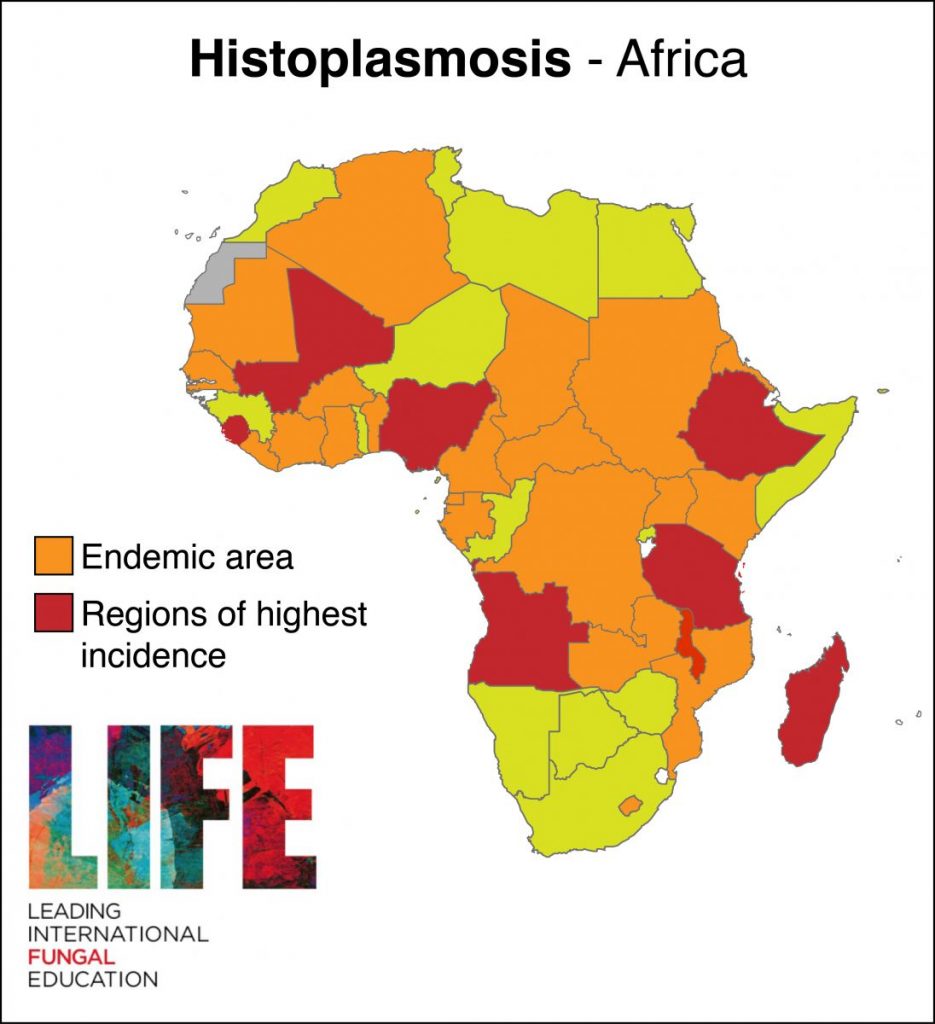
Histoplasma endemicity
Histoplasma capsulatum is endemic to much of Africa (Oladele et al, 2018) and Latin America (e.g. Almeida et al, 2019), as well as the mid-Western US (Benedict & Mody, 2016) and Southeast Asia (Baker et al, 2019; Pan et al, 2012).

Clinical lectures & patient stories

Factsheets
Progressive disseminated histoplasmosis
| OVERVIEW Progressive disseminated histoplasmosis (PDH) varies from an acute to a subacute course. Acute PDH may be rapidly fatal, with diffuse interstitial or reticulonodular lung infiltrates in association with respiratory failure, shock, coagulopathy and multiorgan failure. Subacute PDH usually presents with weight loss, fever and hepatomegaly in association with focal abnormalities such as lymphadenopathy, meningitis, oral or gastrointestinal ulceration, and adrenal insufficiency. |
| FUNGI Histoplasma capsulatum |
| GLOBAL BURDEN The global number of disseminated histoplasmosis cases in AIDS worldwide has been estimated to be 100,000 annually. |
| RISK FACTORS Extremes of age, immunosuppression. PDH is also an AIDS-defining infection (Zanotti et al, 2018). |
| DIAGNOSIS The gold standard is a Histoplasma antigen test in urine, which is positive in >90% of cases. A Wright’s stain on a blood film or bone marrow aspiration may demonstrate intracellular yeasts. Skin, mucosal or lymph node biopsy will also have characteristic intracellular yeasts visible with fungal stains. These yeast forms can be mistaken for Penicillium marneffei, which can produce a similar illness. Culture is usually positive (50-75%) but is slow and can take 10-20 days, occasionally longer. NOTE: the laboratory should be warned of the possibility of Histoplasma as it is a biosafety class 3 pathogen. |
| TREATMENT The treatment of choice is 3 mg/kg intravenous liposomal amphotericin B (AmBisome) for 2 weeks, followed by itraconazole 200-400 mg daily, assuming no drug interaction with rifampicin. For subacute cases, only itraconazole is necessary, unless there is meningitis. TDM is recommended. Early therapy with ART in new AIDS cases is helpful and recommended. |
| OUTLOOK Some patients are extremely ill when they first present. Overall mortality of PDH is 85-100% without treatment, and reduced to <25% with treatment. Around 80,000 deaths annually are predicted when using the most conservative estimates available. |

Disseminated skin lesions. Courtesy of Dr. E. Rodriguez (Argentina) 
Characteristic skin lesion of disseminated histoplasmosis in AIDS, showing central ulceration. May be mistaken for Penicillium/Cryptococcus 
Skin lesion consistent with subacute PDH. Courtesy of Dr. E. Rodriguez (Argentina) 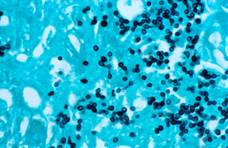
GMS stain showing H. capsulatum in tissue, in context of disseminated histoplasmosis 
Anal ulceration as a manifestation of subacute PDH 
Skin lesions of acute life-threatening PDH 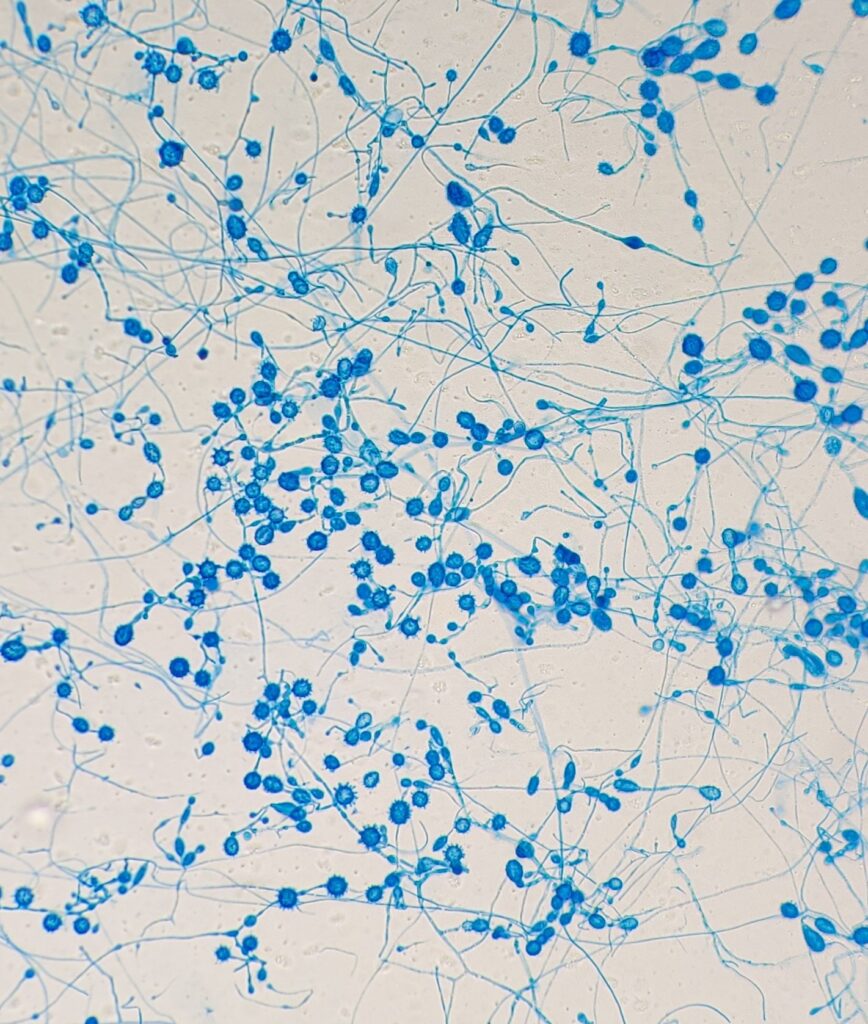
Histoplasma capsulatum. Source: bone biopsy

Acute pulmonary histoplasmosis
| OVERVIEW In acute pulmonary histoplasmosis, most exposed individuals are asymptomatic or have mild self-limiting illnesses. In endemic areas, most people either have positive skin tests or typical radiological features of lymph node or diffuse or multifocal parenchymal calcification, signifying prior exposure which was clinically unrecognised. If exposure is heavy, an acute illness 2-4 weeks after exposure may develop in which fever, myalgia, headache, cough, dyspnoea and chest discomfort predominate. Sometimes arthralgia and/or erythema nodosum occur. Mediastinal lymphadenopathy can be massive. |
| FUNGI Histoplasma capsulatum |
| GLOBAL BURDEN Exposure is common in the areas in which histoplasmosis is endemic but symptomatic disease is uncommon. |
| RISK FACTORS Cavers (spelunkers) and those in the construction industry, doing excavation or demolishing or building new buildings, cleaning chicken coops and heavy outdoor work. The organism thrives in bat and bird guano. The larger the inoculum, the more severe the illness. Primary infection in immunocompromised patients, especially those with advanced HIV infection and taking corticosteroids can be severe and fatal. |
| DIAGNOSIS Seroconversion of antibody in blood is the usual means of making the diagnosis of acute pulmonary histoplasmosis in non-immunocompromised patients. Histoplasma antigen and PCR may also be positive in the acute phase and are important investigations in immunocompromised patients. Culture is occasionally positive but is slow and can take 10-20 days, occasionally longer. NOTE: the laboratory should be warned of the possibility of Histoplasma as it is a class 3 pathogen. |
| TREATMENT Usually none, but if severe illness with high fever and hypoxia then intravenous lipid- associated amphotericin B for 1-2 weeks with oral corticosteroids (e.g. 30 mg prednisolone daily). This should be followed by itraconazole 200 mg twice daily. TDM is recommended. The duration is uncertain, but no less than 12 weeks. |
| OUTLOOK Usually excellent in immunocompetent patients. Rare complications of fibrosing mediastinitis and adrenal dysfunction. |
Massive mediastinal mass of lymph nodes impinging on the oesophagus (see arrows) and affecting swallowing 
Acute pulmonary histoplasmosis in a caver (spelunker)