A recent Indian study has shown that there is no difference in the proportion of patients with chronic pulmonary aspergillosis (CPA) who experience a favourable response following treatment with either itraconazole or voriconazole. The study also found similar rates of relapse in chronic pulmonary aspergillosis across the two groups. However, significantly more adverse events were associated with voriconazole compared with itraconazole.
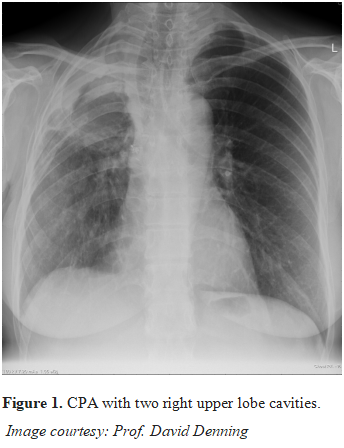
Led by Inderpaul Sehgal of Postgraduate Institute of Medical Education and Research, Chandigarh, this single-centre, prospective, open-label, superiority trial enrolled treatment-naive adults aged 18 years or older with chronic cavitary or chronic fibrosing pulmonary aspergillosis. Participants were randomly assigned 1:1 to receive 200 mg twice daily oral itraconazole or oral voriconazole for 6 months. The primary and secondary outcomes were the proportion of participants achieving a favourable response at 6 months and safety analyses.
Contrasting views were however documented in two previous studies, which showed voriconazole as preferred to itraconazole in the treatment of CPA. While Tashiro et al reported that maintenance therapy with voriconazole was more effective than maintenance therapy with itraconazole in reducing the need for a switch in therapy or hospitalisation following treatment with intravenous antifungal therapies, Al-Shair and colleagues found greater improvement in Saint George’s Respiratory Questionnaire scores with voriconazole than with itraconazole. Sehgal et al in the current study argued that the previous studies were observational and used varying response assessment methods, unequal treatment duration with itraconazole and voriconazole, and a lower median itraconazole dose (200 mg/day) than used in this study. In addition, therapeutic drug monitoring was not routinely performed in the Japanese study. In a prospectively followed cohort of 105 and 27 patients with CPA started on itraconazole and voriconazole respectively, 50% of patients had to change therapy before 12 months for various reasons, usually failure or side effects (Bongomin, 2018).
Conclusively, while both agents may be effective in the treatment of CPA, the combination of clinical failure and toxicity really limits the use of both drugs. Though the findings from this index study support the use of itraconazole as the preferred therapy for CPA, the choice between the two agents should be guided by factors such as patient tolerance, drug availability, and cost considerations.