The incidence of Pneumocystis pneumonia (PCP) has declined significantly in people living with HIV but has steadily been increasing in non-HIV immunocompromised populations including solid-organ transplant (SOT) recipients. Recent studies have it that SOT recipients comprise approximately 30% of HIV-negative PCP cases, mainly in kidney-transplant recipients, often after prophylaxis has been stopped.
Mycophenolic acid (MPA) targets purine biosynthesis and is a key anti-rejection drug for transplantation. MPA also protects against PCP, probably because it interferes with Pneumocystis jirovecii purine biosynthesis. A recent increase in PCP in those taking MPA was documented and the possible mechanisms underlying this shift have been reported in recent studies.
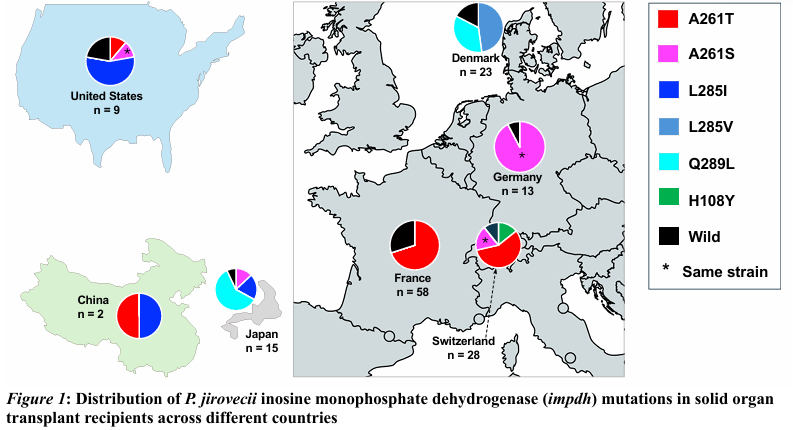
A study from France, examining PCP in SOT patients, linked a nonsynonymous mutation (A261T) in the P. jirovecii inosine monophosphate dehydrogenase (IMPDH) gene to prior therapy with MPA. Further genotyping studies showed that the A261T mutation was associated with a single P. jirovecii strain [Hoffmann et al. 2021], suggesting that MPA exposure led to the selection of a specific P. jirovecii strain, which then circulated among SOT recipients.
More insights into this are demonstrated in a recent international multicenter retrospective observational study by Liang Ma et al in which the P. jirovecii IMPDH gene from samples collected from 96 SOT patients (94 from nine separate outbreaks and 84 on MPA therapy) and 67 non-transplant controls (none on MPA) were sequenced and computational modeling deployed to predict the effects of IMPDH mutations on protein structure and MPA binding. Six mutations (H108Y, A261T, A261S, L285I, L285V, and Q289L) in the P. jirovecii IMPDH gene were identified of which five (A261T, A261S, L285I, L285V, and Q289L) were strongly associated with SOT status and MPA exposure. This study also revealed that four of the six mutations were each linked to multiple distinct strains and with structural modeling, four mutations were predicted to reduce protein stability and binding affinity to MPA.
Studies have demonstrated Pneumocystis jirovecii infections occur in SOT recipients with rates of 0.3%–2.6% [Iriat et al. 2015]. The rates vary with the type of transplantation and are reportedly greater in heart-, lung-, and combined heart–lung transplantation than in kidney- or liver-transplant recipients, regardless of whether they do or do not receive prophylaxis [Iriat et al. 2015].
