Clinical videos
Otomycosis.wmv
MOST CHALLENGING Otomycosis Fungal Ear Infection Removal from Ear with Glue Ear – #370
OTOMYCOSIS

Factsheet
| NAMES Otitis externa; otomycosis; fungal ear infection |
| DISEASE A subacute or chronic superficial fungal infection of the external auditory canal and auricle. Common symptoms include itching, irritation, discomfort, pain and scanty discharge from the affected ear. Usually only one ear is affected. There is also a feeling of blockage in the ear due to collection of debris material in external auditory canal. Irritation is more marked in fungal as compared to bacterial otitis externa. |
| FUNGI Aspergillus niger; A. flavus; A. fumigatus; Scedosporium apiospermum and various species of Candida (including C. auris). |
| GLOBAL BURDEN Otitis externa is common: the acute form affects 1/250 persons annually, while the chronic form affects 3-5% of the population (200-350 million). Acute disease commonly results from bacterial (90%) or fungal (10%) overgrowth in an ear canal subjected to excess moisture or to local trauma. |
| RISK FACTORS A. niger is usually a secondary invader of tissue already rendered susceptible by bacterial infection, physical injury or excessive cerumen (earwax) in the external auditory canal. Invasive external otitis invading continuous bone, and even brain, occurs in both immunocompromised and non-immunocompromised patients. |
| DIAGNOSIS Microscopy and culture of debris collected from the external auditory canal. |
| TREATMENT Careful drying and cleaning of external auditory canal preferably by suction evacuation. Syringing of external auditory canal should be avoided. Topical therapy with antifungal or other antimicrobial such as econazole (1%) solution (very effective), amphotericin B (3%), flucytosine (10%), clotrimazole cream, powder or solution (1%), thiomersal (Merthiolate) or Cresyl acetate solution. Salicylic acid, griseofulvin and ketoconazole are less effective. 4% boric acid solution in alcohol and frequent suction cleaning of the ear canal is a cost-effective treatment. Treatment should continue for 1-3 weeks. Oral antifungal therapy is only required if patients fail topical therapy or have invasive external otitis. |
| OUTCOMES With good ear canal cleaning and antifungal therapy, otomycosis is usually cured and does not relapse. Rarely, A. fumigatus may cause invasive external otitis (also called necrotizing or malignant otitis externa) with local spread to bone and cartilage, a severe and potentially life-threatening disease. |
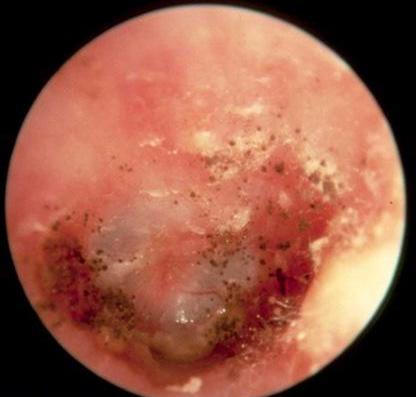
Another greatly magnified example showing an inflamed external auditory canal, with some debris and some sporulating A. niger. (from Miroslava Pőczová) 
A more typical and less distinctive appearance of severe otitis externa, showing much debris, which requires removal 
Typical magnified appearance in the ear canal of moderately severe otitis externa. The black dots are sporulating A. niger colonies. (from Osguthorpe & Nielsen, 2006)
