A new study by Liu et al has documented 114 cases of invasive candidiasis from a recent single-centre, retrospective analysis of patients with infected pancreatic necrosis. Of these, 60.5% had candidemia with or without pancreatic fungal infection, and 39.5% had isolated pancreatic fungal infection. Mixed fungal-bacterial co-infections were identified in 43.9 % of fungal-positive specimens. This is by far the highest reported candidal infection rate in patients with fungal pancreatic infections compared with previous studies such as Rasch et al and Reuken et al, which reported 61 and 49 cases of invasive candidiasis, respectively.
Of the 129 Candida strains isolated in this study, Candida albicans accounted for only 26.36%. Other causative species were Candida parapsilosis complex (21.7 %), Candida tropicalis (20.9 %), and Candida glabrata complex (17.8 %). Echinocandins were mostly used for treatment (68.4 %), followed by azoles (31.6 %), while a minority of patients (14.0 %) received combination antifungal therapy. Fluconazole and voriconazole susceptibility rates of 60.7 % and 75.0 %, respectively, for C. parapsilosis was lower compared with other Candida species.
The authors aimed to identify factors associated with antifungal therapy failure and mortality in infected pancreatic necrosis complicated by invasive candidiasis. Antifungal therapy was effective in 38.6 % of patients on day 7 and in 63.2 % at the end of intravenous treatment. Septic shock, intra-abdominal hemorrhage, breakthrough fungal infection, and concurrent bacterial infection were significantly associated with antifungal therapy failure on day 7, while breakthrough fungal infection alone was identified as an independent risk factor for overall antifungal therapy failure on day 7.
On the other hand, variables significantly associated with antifungal therapy failure at the end of intravenous treatment were septic shock, multiple organ dysfunction syndrome, empirical antifungal therapy and concurrent bacterial infection.
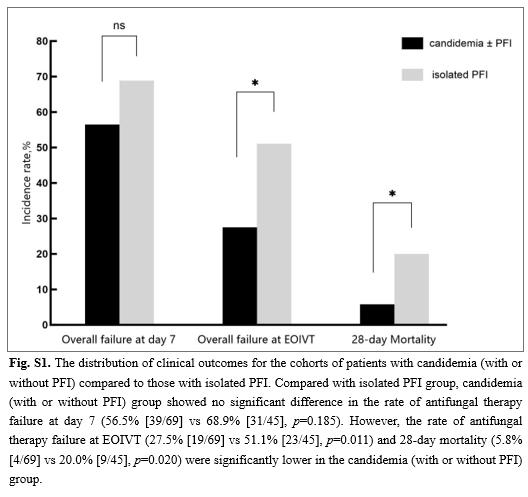
Overall, the study reported a remarkably low mortality rate of 11.4% amongst participants with invasive candidiasis, but with higher values documented for participants with septic shock and multiple organ dysfunction syndrome. In addition, mortality was higher in cases with isolated pancreatic fungal infection (69.2%) compared with candidemia with or without pancreatic fungal infection (30.8%) which is consistent with reports that deep-seated invasive candidiasis generally yields lower success rates than candidemia.