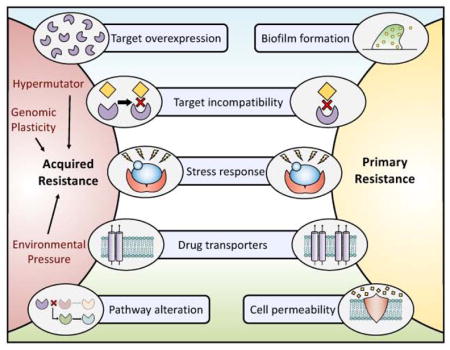
Antifungal resistance is an important cause of treatment failure.
For detailed reviews of the mechanisms underlying resistance please see Perlin et al (2017), Cowen et al (2015) or Revie et al (2018).

Breakpoints & susceptibility testing
Resistance can be either MICROBIOLOGICAL (intrinsic resistance or acquired ie presence of a resistance mutation) or CLINICAL (treatment failure). Examples of intrinsic resistance include: Aspergillus and fluconazole, Candida krusei and Aspergillus terreus and amphotericin B, Cryptococcus and Mucorales and echinocandins.
EUCAST publishes lots of useful information for susceptibility testing, including validated methods, breakpoint tables for Aspergillus and Candida, and provides guidance for other organisms.
Intermediate resistance
Empirical antifungal therapy and prophylaxis save lives, but may be associated with the development of antifungal resistance.
Candida parapsilosis Y132F (Choi et al, 2018)

Antifungal stewardship
IDSA/SHEA provide guidance in setting up a stewardship programme (Dellit et al, 2007; updated by Barlam et al, 2016).
A free online course is available via FutureLearn, : Role of Antifungal Stewardship
Reviewed by (Hamley et al, 2017)
The cornerstones of an antifungal stewardship programme are:
- Rapid diagnostics, including susceptibility testing
- TDM
- Targeted (i.e. not empirical) prescribing of antifungals
- Check whether your hospital includes antifungals in its site-wide antibiogram

